POSSIBLE SIDE EFFECTS AND RISKS
- ourservices
POSSIBLE SIDE EFFECTS AND RISKS
Possible side effects of injectable fertility medicines include
- Mild bruising and soreness at the injection site (using different sites for the injections can help)
- Nausea and, occasionally, vomiting
- Temporary allergic reactions, such as skin reddening and/or itching at the injection site
- Breast tenderness and increased vaginal discharge
- Mood swings and fatigue
- Ovarian hyperstimulation syndrome (OHSS)
Most symptoms of OHSS (nausea, bloating, ovarian discomfort) are mild. They usually go away without treatment within a few days after the egg collection. In severe cases, OHSS can cause large amounts of fluid to build up in the abdomen (belly) and lungs. This can cause very enlarged ovaries, dehydration, trouble breathing, and severe abdominal pain. Very rarely (in less than 1% of women having egg retrieval for IVF), OHSS can lead to blood clots and kidney failure. For more information about OHSS, see the ASRM fact sheet Ovarian hyperstimulation syndrome (OHSS).
Earlier reports from several decades ago suggested a link between ovarian cancer and the use of fertility medicines. However, more recent and well done studies no longer show clear associations between ovarian cancer and the use of fertility medications.

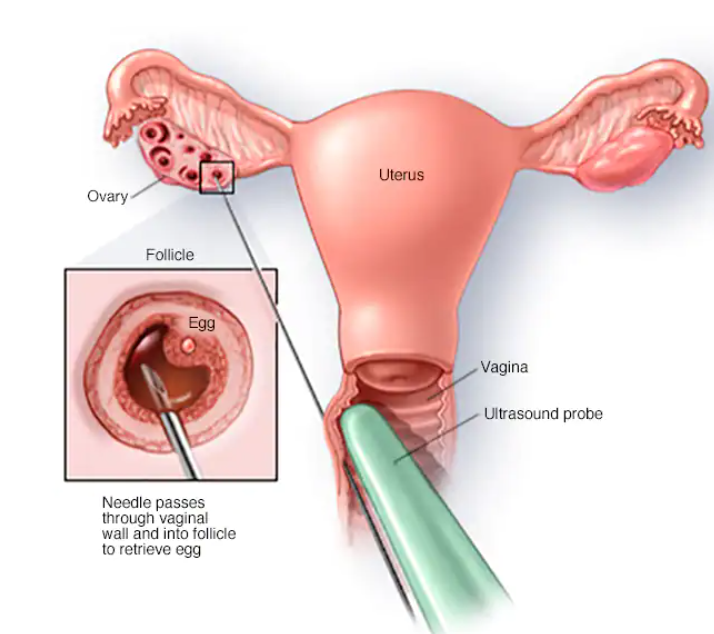
What are the risks of the egg retrieval?
During the egg retrieval, your doctor uses vaginal ultrasound to guide the insertion of a long, thin needle through your vagina into the ovary and then into each follicle to retrieve eggs. Possible risks for this procedure include:
- Mild to moderate pelvic and abdominal pain (during or after). In most cases, the pain disappears within a day or two and can be managed with over-the-counter pain medications.
- Injury to organs near the ovaries, such as the bladder, bowel, or blood vessels. Very rarely, bowel or blood vessel injury can require emergency surgery and, occasionally, blood transfusions.
- Pelvic infection (mild to severe). Pelvic infections following egg retrieval or embryo transfer are now uncommon because antibiotic medicines are usually given at the time of egg collection. Severe infection may require hospitalization and/or treatment with intravenous antibiotics.
- Rarely, to manage a severe infection, surgery may be required to remove one or both of the ovaries and tubes and/or uterus. Women who have had pelvic infections or endometriosis involving the ovaries are more likely to get IVF-related infections.
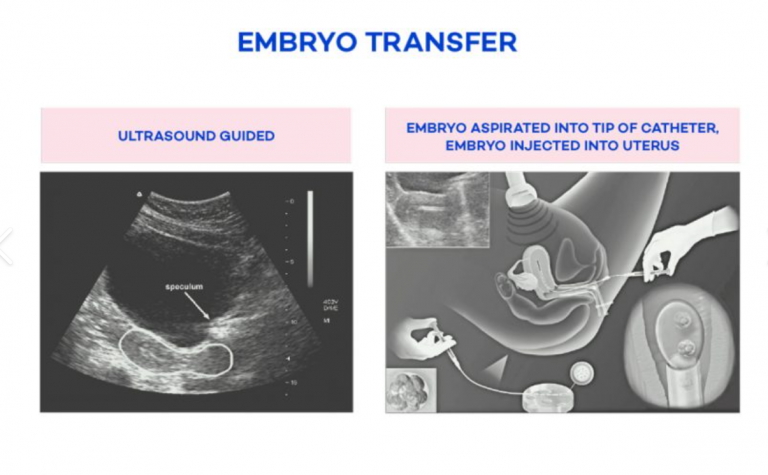
What are the risks associated with the embryo transfer?
A catheter containing the embryos is used to gently place them into the uterus (womb). Women may feel mild cramping when the catheter is inserted through the cervix or they may have vaginal spotting (slight bleeding) afterward. Very rarely, an infection may develop, which can usually be treated with antibiotics.
If I conceive with IVF, will my pregnancy be more complicated (than if I conceived on my own)?
Having a multiple pregnancy (pregnancy with more than one baby) is more likely with IVF, particularly when more than one embyro is transferred. These pregnancies carry significant risks, including:
- Preterm labor and/or delivery: premature babies (regardless of whether or not they were conceived naturally or with IVF) are at higher risk for health complications such as lung development problems, intestinal infections, cerebral palsy, learning disabilities, language delay, and behavior problems
- Maternal hemorrhage
- Delivery by cesarean section (C-section)
- Pregnancy-related high blood pressure
- Gestational diabetes
The more embryos that are transferred into the uterus, the greater the risk. Your doctor should transfer the minimum number of embryos necessary to provide a high likelihood of pregnancy with the lowest risk of multiple pregnancy. For more information about multiple pregnancy, see the ASRM booklet titled Multiple pregnancy and birth: twins, triplets and highorder multiples. One way to avoid multiple pregnancy is to choose to transfer only one embryo at a time. For more information about this, see the ASRM fact sheet Single embryo transfer.
Will IVF increase the risk of my child having a birth defect?
The risk of birth defects in the general population is 2%-3%, and is slightly higher among infertile patients. Most of this risk is due to delayed conception and the underlying cause of infertility. Whether or not IVF alone is responsible for birth defects remains under debate and study. However, when intracytoplasmic sperm injection (ICSI) is done along with IVF, there may be an increased risk of birth defects.
In addition, there may be a slight increased risk of sex chromosome (X or Y chromosome) abnormalities with ICSI. However, it is uncertain if these risks are due to the ICSI procedure itself or to problems with the sperm themselves. Men with sperm defects are more likely to have chromosomal abnormalities, which can be transmitted to their children. However, these disorders are extremely rare. Rare genetic syndromes called imprinting disorders may be slightly increased wtih IVF.
Miscarriage and ectopic pregnancy
The rate of miscarriage after IVF is similar to the rate following natural conception, with the risk going up with the mother’s age. The rate of miscarriage may be as low as 15% for women in their 20s to more than 50% for women in their 40s.
There is a small risk (1%) of an ectopic (tubal) pregnancy with IVF; however, this rate is similar to women with a history of infertility. If an ectopic pregnancy occurs, a woman may be given medicines to end the pregnancy or surgery to remove it. If you are pregnant and experience a sharp, stabbing pain; vaginal spotting or bleeding; dizziness or fainting; lower back pain; or low blood pressure (from blood loss), and have not had an ultrasound confirming that the pregnancy is in the uterus, call your doctor immediately. These are all signs of a possible ectopic pregnancy. There is a 1% risk for a heterotopic pregnancy after IVF. This is when an embryo implants and grows in the uterus while another embryo implants in the tube, leading to a simultaneous ectopic pregnancy. Heterotopic pregnancies usually require surgery (to remove the ectopic pregnancy). In most cases, the pregnancy in the womb can continue to develop and grow safely after the tubal pregnancy is removed.